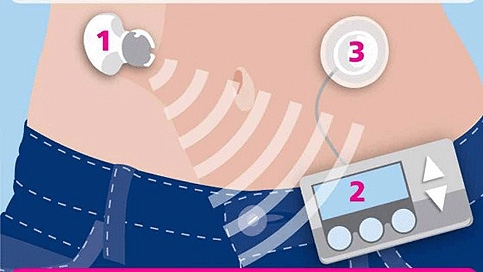
The system uses a small subcutaneous patch to continuously monitor glucose levels, sending the results via radio frequency to a small computer that calculates the appropriate insulin dose, which is then delivered by a insulin pump.
‘The system has the potential to improve the safety and effectiveness of insulin delivery and may allow more flexible lifestyles in the future,’ said Dr Roman Hovorka of Cambridge University, who led the study.
He added that it could be particularly useful when worn at night, since this is the time when most patients experience potentially dangerous blood-sugar drops — or hypoglycemic events — which are also exacerbated by alcohol consumption.
The conventional approach to diabetes monitoring and treatment is based around finger-prick testing combined with daily insulin injections that are adjusted accordingly by the patient with help from health workers.
In recent years, several technologies have started to come through to help patients better manage their condition around their daily activities.
Indeed, several non-invasive patches that can be worn discreetly to continuously monitor blood sugar are now available. Meanwhile, insulin pumps, which are the size of a mobile phone and can be worn on a belt, have been developed to deliver a more steady dose over the course of the day. However, these still require input and co-ordination from patients or clinicians, with the potential for errors or simple forgetfulness.
What the team did was to connect these technologies in a closed-loop system that it likens to an ‘artificial pancreas’. By designing algorithms to interpret blood-glucose signals and deliver the appropriate dose, it hoped to achieve completely autonomous monitoring and dose delivery.
’The point of this was to test the devices in different real-world situations,’ Hovorka said of the subsequent clinical trial.
It was worn by 12 diabetics overnight after they had consumed a large meal with 100g of carbohydrate accompanied by alcohol at 8.30pm. There was a 22 per cent improvement in the time participants kept their blood-glucose levels in a safe range and a halving of the number of incidents of low blood-glucose levels.
‘Closed-loop systems may serve as a bridge until diabetes is cured by, for example, stem-cell therapy or islet transplantation,’ Hovorka said.





Nanogenerator consumes CO2 to generate electricity
Whoopee, they've solved how to keep a light on but not a lot else.