A novel take on the concept of video endoscopy could improve detection of cancer in the throat and digestive system. Developed at Glasgow University, the technique uses a diagnostic technique that was previous too bulky to be installed in a swallowable device.
Video endoscopy is a technology that is still in its early stages, using a very small video camera with integrated lighting and electronic transmission all encapsulated into a capsule small enough for a patient to swallow and to travel through the digestive system sending back images to a clinician. It is being developed to detect cancers, injuries and lesions within the digestive system without the need for the often-traumatic technique of endoscopy, where a camera on the end of a flexible, steerable rod is inserted into the patient’s throat or rectum to image the upper or lower gastrointestinal duct. But even with its undoubted potential, video endoscopy is limited: it can only detect what can be seen using visible light.
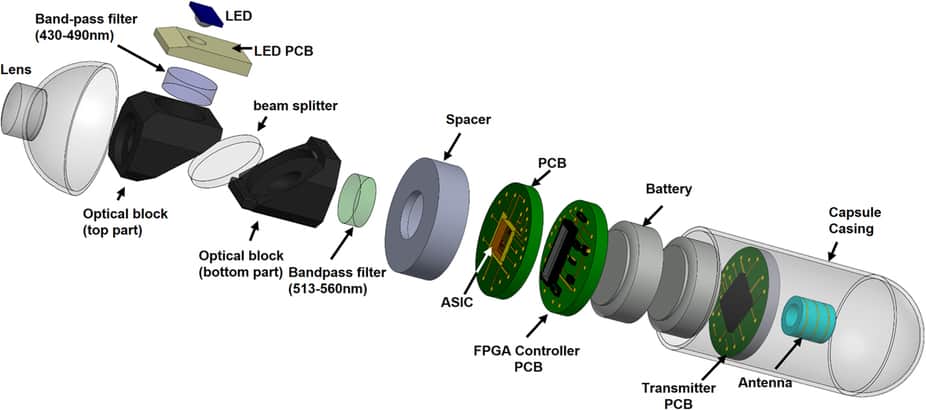
The Glasgow team, led by Prof David Cumming, have combined video endoscopy with a technique called fluorescence imaging, which exploits a phenomenon where certain molecules emit light when they are illuminated by specific wavelengths outside the visible spectrum. Fluorescence imaging has previously needed very large equipment that consumes a lot of power, and has therefore been restricted to use on surgically-removed samples in a laboratory. Cummings’ team, which specialises in electronic and nanoscale engineering, has devised a miniaturised version using an advanced semiconductor single-pixel imaging technique, which they describe in a paper in the journal Scientific Reports. The crucial component, a single-photon avalanche detector (SPAD), generates a pulse of current every time it is hit by a photon of the fluorescent light, which is generated using a simple LED to illuminate the suspected tumour. ‘The system we’ve developed is small enough and power efficient enough to image the entire human gastrointestinal tract for up to 14 hours,’ said research associate Dr Mohammed Al-Rawhani.
Testing has so far been in vitro only. ‘We’ve confirmed in the lab the ability of the system to image fluorescence ‘phantoms’ – mixtures of flavins and haemoglobins which mimic closely how cancers are affected by fluorescence in parts of the body like the intestines, the bowel and the aesophagus,’ said Al-Rawhani. ‘The system could also be used to help track antibodies used to label cancer in the human body, creating a new way to detect of cancer,’ he added.
Cumming also stressed that the system is not ready for the clinic. ‘There’s still some way to go before it will be ready for commercial production and clinical use, but we’re in early talks with industry to bring a product to market,’ he said. ‘We’re also interested in expanding the imaging capabilities of video-pill systems to new areas such as ultrasound in the near future.’




April 1886: the Brunkebergs tunnel
First ever example of a ground source heat pump?