 Andrew Wade, senior reporter
Andrew Wade, senior reporter
The science of cryonics is in the spotlight after a 14-year-old girl won the right to have her body frozen, the judgement coming shortly before she died of cancer. It’s yet another example of how science and technology are testing our legal and ethical boundaries, and how governments and institutions are struggling to keep pace.
Known only in legal documents as ‘JS’, the girl was represented in court by her mother, who was fighting for her daughter’s right to be preserved and transported from London to the US and frozen “in perpetuity”. The cost for this cryopreservation is being reported as £37,000, a sum raised by the mother’s parents, according to the judge. And while honouring a dying child’s wishes may have immeasurable value, the case raises questions as to the scientific viability of cryonics, and the ethical validity of the multimillion dollar industry that has grown up around it.

Delivering his judgment, Mr Justice Peter Jackson weighed up the merits of the arguments.
“The scientific theory underlying cryonics is speculative and controversial, and there is considerable debate about its ethical implications,” he said. “On the other hand, cryopreservation, the preservation of cells and tissues by freezing, is now a well-known process in certain branches of medicine, for example the preservation of sperm and embryos as part of fertility treatment. Cryonics is cryopreservation taken to its extreme.”
Essentially, we simply don’t know if cryonics works. Scientific advances have allowed us to successfully freeze sperm and embryos for fertility treatment, as well as blood cells and small amounts of tissue. However, scaling up to more complex cell combinations is difficult, and we are yet to develop the ability to cryopreserve human organs, something that would revolutionise transplant medicine and open the door to full body cryonics.
“If they are to survive, frozen cells are not ‘frozen’ - they must contain no ice crystals, which would otherwise invariably kill them,” said Barry Fuller, professor in surgical science & low temperature medicine at University College London.
As many mountaineers and polar explorers can attest, cells don’t react well to being frozen and thawed, their walls breaking down when ice crystals form. Cryopreservation overcomes this through vitrification, where a combination of antifreeze-type chemicals and careful reduction of temperature is used to harden cell material into a glass-like state.

“Cryopreservation has not yet been successfully applied to large structures, such as human kidneys for transplantation, because we have not yet adequately been able to produce suitable equipment to optimise all the steps,” said Fuller.
“This is why we have to say that at the moment we have no objective evidence that a whole human body can survive cryopreservation with cells which will function after rearming.”
The case of JS was unusual for several reasons, not least the complications arising from the girl’s age. Fulfilling her wishes required the cooperation of the local hospital trust, which faced “serious legal and ethical issues” according to the judge. Indeed, although the trust helped out in this instance, Justice Jackson noted that “all the professionals feel deep unease about it.”
Medical staff finding themselves in such a predicament is indicative that clearer regulation is required, and it looks like steps are being taken in the right direction. The Human Tissue Authority (HTA) - which regulates organisations that remove, store and use human tissue – was contacted in relation to this case, but claimed it had no remit to act. However, it says cryopreservation is an area it is monitoring closely in conjunction with the Department of Health, and one where there is “the possible need for regulatory oversight.”
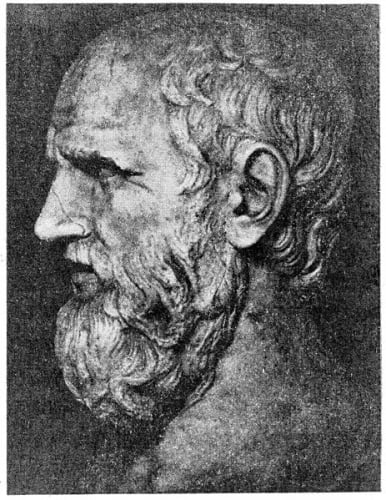
Healthcare and ethics have long been intertwined, stretching back to the days of Hippocrates and beyond. As such, there is an established ethical framework that has grown up around medicine, and scientific advances are generally subject to stringent regulations and certification. But the rapid progress being made in other sectors is unearthing ethical conundrums with no precedent.
Autonomous vehicles raise questions around agency, ownership, and utilitarianism; how does a vehicle AI choose between potentially killing its ‘driver’, or potentially killing multiple pedestrians? The evolution of robotics and automation has ominous implications for global employment, with low-skilled labour likely to suffer. And above all, machine learning and AI has been identified by several leading scientists as potentially the biggest threat to the existence of humanity. Addressing these issues will not be easy, but burying our heads in the sand is not an option. Genies are escaping their bottles and cannot be put back in. Governments must take steps to guide them.




Red Bull makes hydrogen fuel cell play with AVL
Formula 1 is an anachronistic anomaly where its only cutting edge is in engine development. The rules prohibit any real innovation and there would be...