An improvement in the ability of clinicians to diagnose cancer and to understand how it spreads through the body could result from a new technique that uses sound waves to isolate cancer cells in blood samples. Developed by engineers from Penn State University, Carnegie Mellon University and MIT, the ‘acoustic tweezers’ will give doctors a low-cost method of separating cancer cells without damaging them.
In blood samples from cancer patients, typically one cell in a billion is a circulating cancer cell (CTC). “Looking for CTCs is like looking for a needle in a haystack,” said research leader Tony Jun Huang.
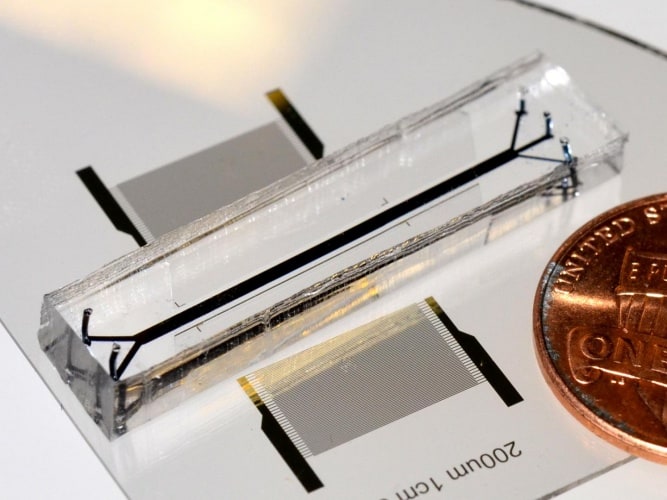
The acoustic tweezers use a phenomenon called tilted-angle surface acoustic waves to separate out tumour cells. This is much gentler than centrifugation, which spins the sample at 3,000rpm for ten minutes. The team used a microfluidic device to analyse the blood samples continuously, and chose acoustic pressures that would nudge the CTCs, which are heavier than blood cells, out of the stream and into a collection channel.
The technique works by placing two sound sources on either side of the flow, emitting the same wavelength: this creates a region where the two sounds cancel each other out, and the sources are positioned so that this ‘neutral zone’ is in the collection channel. The technique uses very small amounts of energy — about the same as that used for ultrasonic imagery, which is known to not damage cells — and does not require cell labelling.
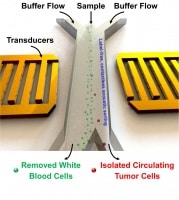
The team used two types of cultured human cancer cell to test the technique, and achieved a separation rate of 83 per cent.
“Because these devices are intended for use with human blood, they need to be disposable,” Huang said in a statement. “We are currently figuring out manufacturing and mass production possibilities.”
Another member of the research team, Subra Suresh of Carnegie Mellon, said the technique “promises to offer new avenues for basic research into the pathology and metastasis, and for clinical diagnosis of rare tumor cells.”




Project to investigate hybrid approach to titanium manufacturing
What is this a hybrid of? Superplastic forming tends to be performed slowly as otherwise the behaviour is the hot creep that typifies hot...