For many diabetics, regular monitoring of blood glucose is simply a part of staying healthy; and that means firing a sharp, spring-loaded pin into your finger to obtain a blood sample several times a day. It’s not incredibly painful, but it’s nobody’s idea of a pleasant experience and it’s to say the least an inconvenience. Non-invasive blood testing methods have been a goal of researchers for years; and a group in China now claims to have developed just such a system.
The multidisciplinary group, from Tsinghua University in Beijing, has developed a multilayered biosensor in the form of a thin film that can be simply stuck to the skin, and used in conjunction with electronics to provide an accurate measurement of blood glucose levels. The measurement process, described in Science Advances, has several stages.
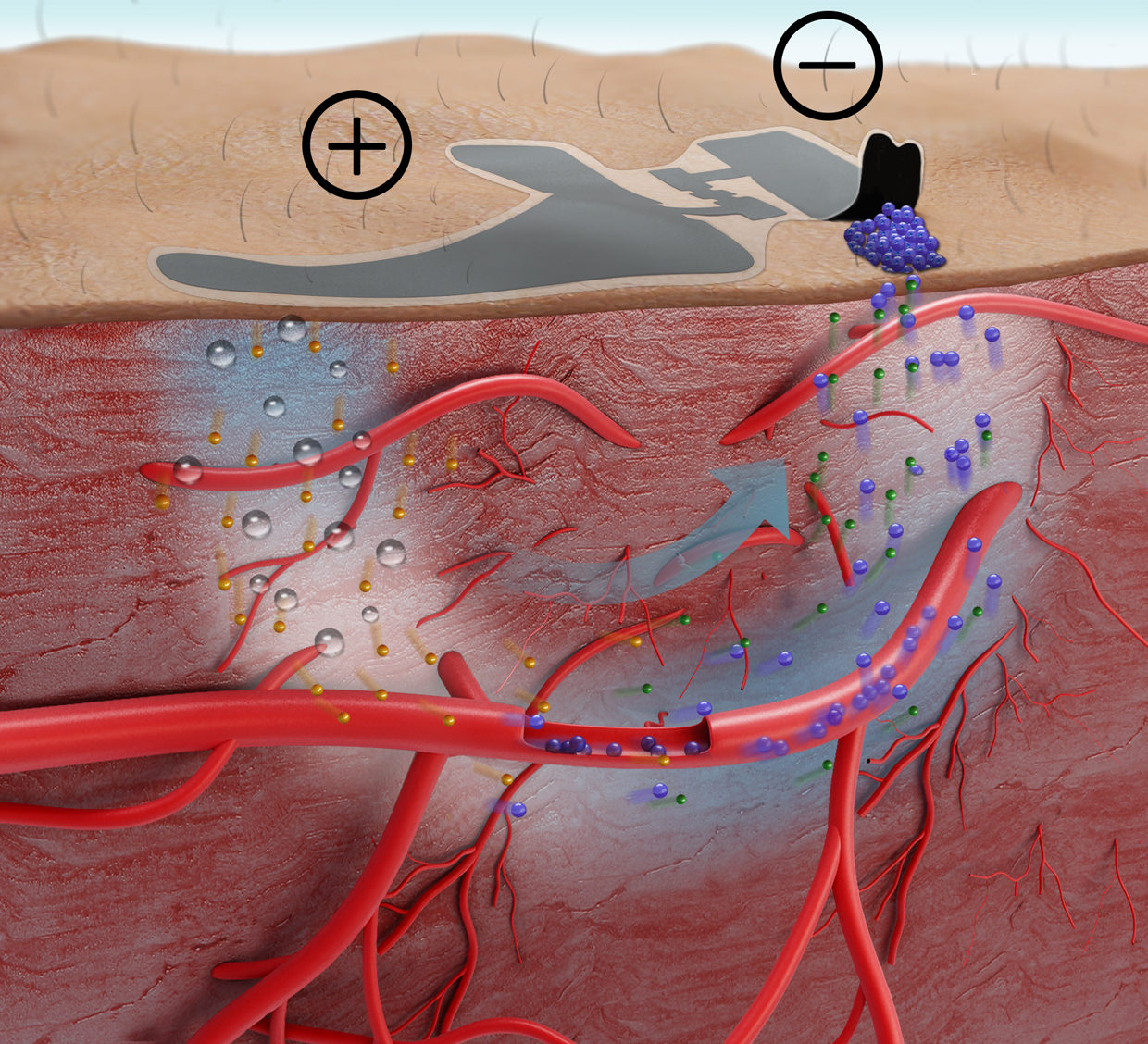
First, the user attaches a paper battery to the location where the measurement is to be taken; this creates an electrical potential gradient in the tissue below the battery. Then, hyaluronic acid (a very common ingredient is moisturisers) must be applied to the battery’s anode; this pushes the positively-charged portion of the acid into the skin. This affects the blood vessels that lie just below the surface, causing them to release glucose, which rises through the skin and collects at he battery’s cathode. After 20 minutes, the battery can be removed and the sensor patch itself stuck to the skin in its place.
The patch is a construction of five layers. In contact with the skin is an 80nm-thick sheet of polymethyl methacrylate, on top of which is a 1.6µm thick layer of polyimide. This is topped by a 100nm thick layer of nanostructured gold film, followed by an electrochemically-deposited nanometre transducer layer and a film containing immobilised glucose oxidase enzymes. The whole film is 3 µm thick and flexible enough to conform with the ridges on the skin, maximising the surface area through which it can measure.
The layers of the sensor film absorb the glucose and convert it into an electrical signal that can be read using standard laboratory equipment. The accuracy is similar to that achieved by finger-stick testing, and the same site can be used an unlimited number of times — although a fresh battery and sensor strip are needed for each test. The lead author of the study, PhD student Yihao Chen, said he is working on incorporating a voltage source and sensor into a closed-loop system with an insulin pump that would effectively form an artificial pancreas.





Red Bull makes hydrogen fuel cell play with AVL
Many a true word spoken in jest. "<i><b>Surely EVs are the best solution for motor sports</b></i>?" Naturally, two electric motors demonstrably...