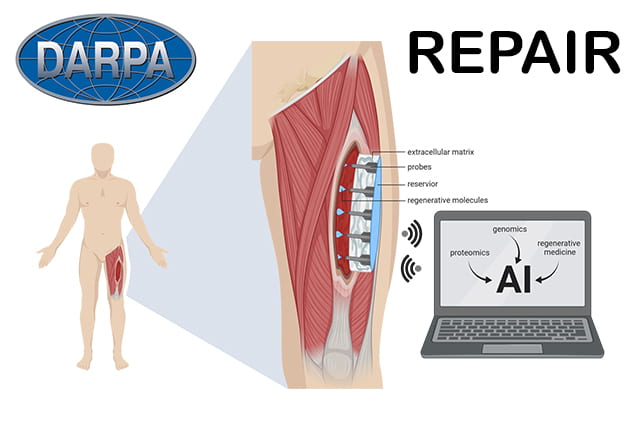
Led by researchers at the University of Pittsburgh, the team will spend the next four years working on REPAIR, an acronym made from REgenerative electronic Patch through Advanced Intelligent Regulation. The project includes researchers from Carnegie Mellon University, Northwestern University, the University of Vermont, the University of Wisconsin, the Walter Reed National Military Medical Center in Maryland, and neuroengineers and bioengineers at Rice University in Texas.
Digital bandage treats chronic wounds
According to Rice, few treatment options exist when trauma destroys over 20 per cent of a muscle. Such large wounds, which are common in recent military conflicts, overwhelm the body’s natural capacity to regenerate muscle tissue. Instead, a stiff scar forms in place of the missing muscle, which can lead to significant disability.
“With these severe injuries it’s been drilled into us through all of our training that functional muscle replacement is not possible,” said grant principal investigator Dr Stephen Badylak, a professor of surgery at the University of Pittsburgh School of Medicine and deputy director of Pitt’s McGowan Institute for Regenerative Medicine. “The sort of technology we’re developing offers hope where there otherwise would have been no hope.”
Badylak envisions creating a device that would change the environment inside larger wounds to help them heal the way smaller wounds do naturally.
Smaller, self-healing wounds typically switch from inflammatory to anti-inflammatory conditions a couple of weeks after the initial injury. Badylak and colleagues imagine inducing larger wounds into anti-inflammatory mode three or four days after an injury, and again a few days later, repeating the cycle until the muscle rebuilds itself.
All of that would be accomplished by REPAIR, a smart device implanted inside the wound. REPAIR will monitor key molecular signals at each stage of healing — from the first hours after injury to the days and weeks that follow — and deliver specific molecules at specific times under the direction of artificial intelligence.
Regrow muscle
Rice will help create bioelectronics for sensing and stimulating biochemical and biophysical factors that regulate wound healing, said lead Rice co-PI Jacob Robinson.
Rice co-PI Ashok Veeraraghavan will lead efforts to create imaging technologies to measure blood flow and vascularisation. Robinson’s team will help with the photonic integration of the imaging technology and develop flexible photonic devices that will be integrated into the intelligent bandage to monitor temperature and biochemical factors in the wound bed.
The first two years of the project will involve developing the device. The next two years will reportedly involve close collaboration with surgeons at Walter Reed, who treat patients with major muscle loss, to refine the design so it’s suitable for clinical use.
The researchers will work with industry partners and the US Food and Drug Administration to identify and clear regulatory hurdles that might slow down clinical translation.
“We’re developing the science and the device in mostly an academic setting,” Badylak said in a statement. “If that’s done without consideration of regulatory and industry requirements, patients would never see it because it would remain buried in institutions with no clear path for clinical translation.”
The REPAIR project to regrow muscle is funded through DARPA’s Bioelectronics for Tissue Regeneration program.





Red Bull makes hydrogen fuel cell play with AVL
Formula 1 is an anachronistic anomaly where its only cutting edge is in engine development. The rules prohibit any real innovation and there would be...