The advance, led by the Georgia Institute of Technology (Georgia Tech) and reported in ACS Nano, has been shown to accurately measure fluid flow in animal blood vessels in vitro. The team is now working on a wireless system that could allow in vivo testing.
Brain aneurysms occur due to a weakness in the wall of a cerebral artery which causes a localised ballooning of the blood vessel. A recent advance in aneurysm treatment is the development of flow diverter devices, which place a porous stent across the neck of an aneurysm to disrupt the intra-aneurysmal flow.
"We have developed a highly stretchable, hyper-elastic flow diverter using a highly-porous thin film nitinol," said Youngjae Chun, an associate professor in the Swanson School of Engineering at the University of Pittsburgh. "None of the existing flow diverters, however, provide quantitative, real-time monitoring of hemodynamics within the sac of cerebral aneurysm. Through the collaboration with… Georgia Tech, we have developed a smart flow-diverter system that can actively monitor the flow alterations during and after surgery."
According to Georgia Tech, flow diverters need to be monitored using MRI and angiogram technology, which is costly and involves injection of a magnetic dye into the bloodstream. The team hope their sensor could provide simpler monitoring in a doctor's surgery using a wireless inductive coil to send electromagnetic energy through the sensor. By measuring how the energy's resonant frequency changes as it passes through the sensor, the system could measure blood flow changes into the sac.
"We are trying to develop a batteryless, wireless device…that can be miniaturised enough to be routed through the tiny and complex blood vessels of the brain and then deployed without damage," said Woon-Hong Yeo, an assistant professor in Georgia Tech's George W Woodruff School of Mechanical Engineering and Wallace H Coulter Department of Biomedical Engineering. "It's a very challenging to insert such electronic system into the brain's narrow and contoured blood vessels."
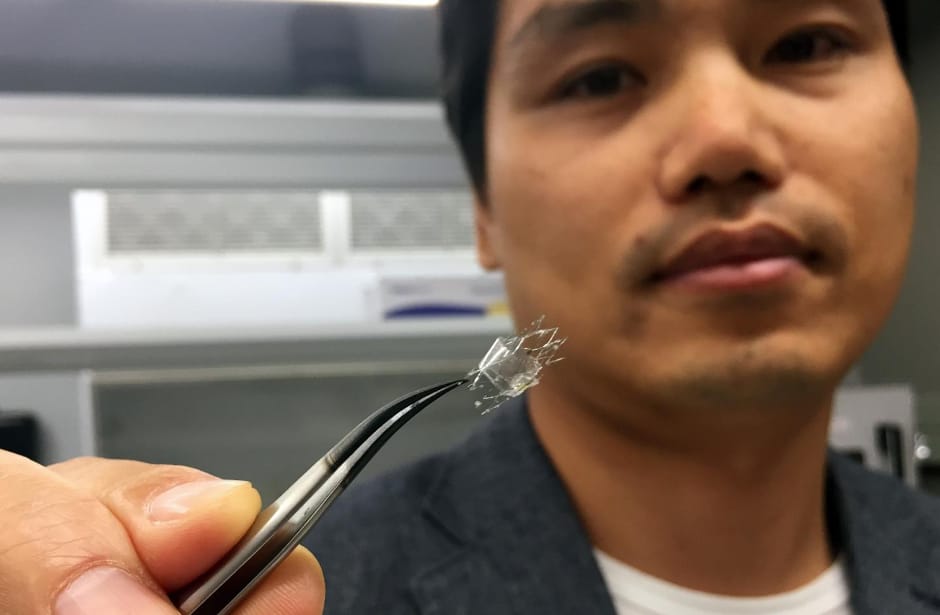
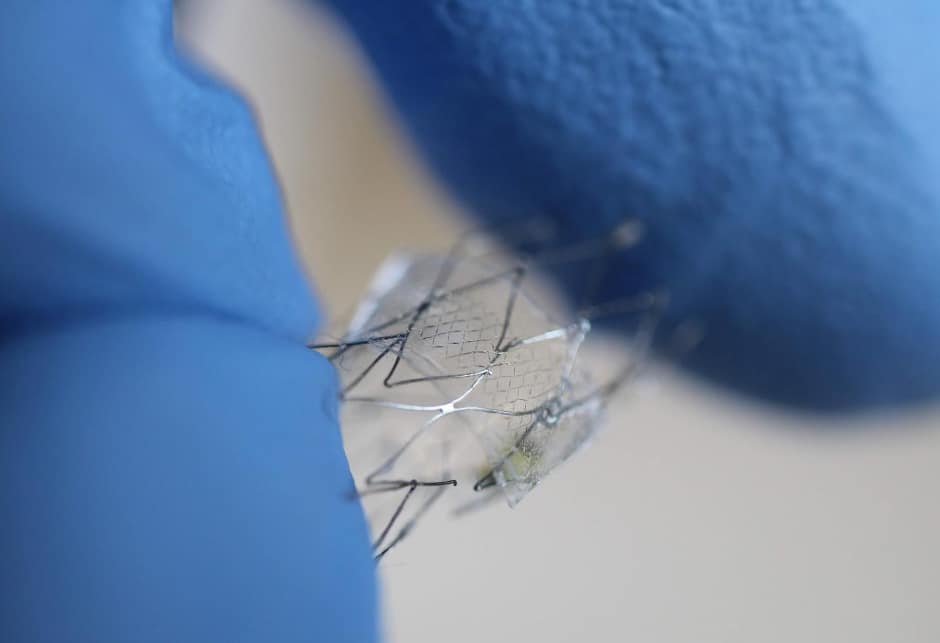
The sensor uses a micro-membrane made of two metal layers surrounding a dielectric material, and wraps around the flow diverter. The device is a few hundred nanometres thick, and is produced using nanofabrication and material transfer printing techniques, encapsulated in a soft elastomeric material.
"The membrane is deflected by the flow through the diverter, and depending on the strength of the flow, the velocity difference, the amount of deflection changes," said Yeo. "We measure the amount of deflection based on the capacitance change, because the capacitance is inversely proportional to the distance between two metal layers."
Because the brain's blood vessels are so small, the flow diverters can be no more than five to ten millimetres long and a few millimetres in diameter. That rules out the use of conventional sensors with rigid and bulky electronic circuits.
"Putting functional materials and circuits into something that size is pretty much impossible right now," Yeo said. "What we are doing is very challenging based on conventional materials and design strategies."
The researchers tested three materials for their sensors: gold, magnesium and the nickel-titanium alloy nitinol. All can be safely used in the body, but magnesium offers the potential to be dissolved into the bloodstream after it is no longer needed.
The proof-of-principle sensor was connected to a guide wire in the in-vitro testing, but Yeo and his colleagues are now working on a wireless version that could be implanted in a living animal model. While implantable sensors are being used clinically to monitor abdominal blood vessels, application in the brain creates significant challenges.
"The sensor has to be completely compressed for placement, so it must be capable of stretching 300 or 400 per cent," said Yeo. "The sensor structure has to be able to endure that kind of handling while being conformable and bending to fit inside the blood vessel."





Swiss geoengineering start-up targets methane removal
No mention whatsoever about the effect of increased methane levels/iron chloride in the ocean on the pH and chemical properties of the ocean - are we...