Most wearable medical devices can measure signals only on the surface of the skin or at very shallow levels below it. However, engineers from the University of California San Diego have now developed a method for using ultrasound in an adhesive patch to monitor blood pressure in deep arteries or veins.
"By integrating ultrasound technology into wearables, we can start to capture a whole lot of other signals, biological events and activities going on way below the surface in a non-invasive manner," said research leader Sheng Xu, a professor of nanoengineering at the Jacobs School of Engineering.

Described in Nature Biomedical Engineering, the device can measure central blood pressure at depths as great as 4 cm below the skin. Central blood pressure is different from the reading taken using an inflatable cuff, which is known as peripheral blood pressure. Central pressure relates to the vessels which carry blood directly from the heart to major organs, and is considered to be a more accurate reading and also better at predicting heart disease.
Normally, measuring central blood pressure is a laborious task, involving inserting a catheter into the arm, groin or neck and guiding it to the heart. The only non-invasive methods currently available, which uses a pen-like probe called a tonometer held in a precise way above a major blood vessel, is very difficult to perform and is not consistently accurate.
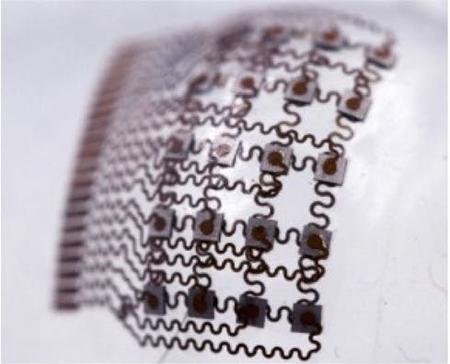
The patch developed by the San Diego team is a thin sheet of a silicone elastomer. Patterned onto this is an array of small electronic components connected by spring shaped wires (this is known as an “island bridge” structure). Each component island contains piezoelectric transducers which produce ultrasound waves when a current passes through them.
These waves penetrate the skin and continuously record the diameter of a blood vessel deep in the body. The diameter changes as blood pulses through it, and the reflected signals are translated into a waveform which is analysed using customised software. The overall shape of the waveform, as well as every feature within it, represents a specific activity or event in the patient’s heart.
The team tested the patch on a male subject who wore it on his forearm, wrist, neck and foot, with readings taken while the subject was stationary and during exercise. The readings were more consistent and precise than recordings taken with the commercial tonometer, the team claims.
"This has the potential to be a great addition to cardiovascular medicine," said Dr Brady Huang, a co-author on the paper and radiologist at UC San Diego Health. "In the operating room, especially in complex cardiopulmonary procedures, accurate real-time assessment of central blood pressure is needed - this is where this device has the potential to supplant traditional methods."
The first author of the paper, nanoengineering postgrad Chonghe Wang, commented: "A major advance of this work is it transforms ultrasound technology into a wearable platform. This is important because now we can start to do continuous, non-invasive monitoring of major blood vessels deep underneath the skin, not just in shallow tissues."
The advanced advantage of the patch and the island bridge structure is that the whole assembly conforms easily to the contours of the part of the body on which it is stuck. However, the team adds that it is not yet suitable for clinical application, because they want to integrate a power source, data processing unit and wireless communications directly into the patch.
"Right now, these capabilities have to be delivered by wires from external devices. If we want to move this from benchtop to bedside, we need to put all these components on board," said Prof Xu. Data processing and wire technology specialists are likely to be involved in the next phase of the research.




Glasgow trial explores AR cues for autonomous road safety
They've ploughed into a few vulnerable road users in the past. Making that less likely will make it spectacularly easy to stop the traffic for...