But ask a person on the street to explain what they are, and you’ll likely get shrugged shoulders.
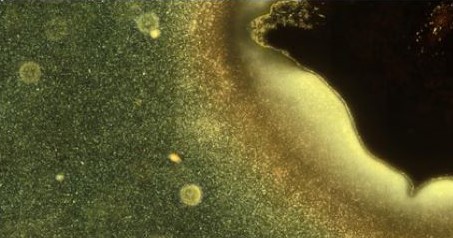
Without realising it, you actually see biofilms everyday – examples include dental plaque, slime on rocks in streams and pond scum.
A biofilm is formed when numerous living microorganisms, such as bacteria or fungi, group together and then evolve and grow as a collective.
Antimicrobial resistance: a call to arms
Biofilms are often detrimental, with biofilm infections estimated to be responsible for up to 80 per cent of all infections in humans and animals.
Gaining a greater understanding of the composition of biofilms and how to prevent, detect, manage and engineer them, would present benefits across a range of sectors, particularly in the healthcare industry where managing infections effectively is a growing issue globally.
To tie in with the National Biofilms Innovation Centre (NBIC)’s #BiofilmAware campaign, The Engineer has teamed up with Loughborough University to explore three areas of research looking to help in the battle against biofilms.
From free-floating microorganisms to biofilm: understanding an important transition that could help tackle medical implant infections
The ability to attach and implant devices in the human body is crucial in modern medicine but a big problem with their use is that they provide a surface for bacteria to colonize on and turn into infectious biofilms.
Loughborough’s Dr Marco Mazza is the group leader of ‘Nonequilibrium Soft Matter’ – a research group trying to understand the early phase in the life of a biofilm, that is, the transition from the very beginning, when there is no biofilm and simply some microbial cells are swimming in a fluid, to the phase when the cells find a surface to colonise, and start reproducing on it.
One of the team’s notable successes is that they discovered a way to monitor biofilm composition and growth while the biofilm forms (paper here) – this is important as it may provide a means for medical professionals to test the response of a biofilm to different treatments that aim to prevent infection.
The researchers are currently exploring different bacterial species and their specific strategies of motion and surface colonisation.
Of the research’s importance, Dr Mazza said: “Microbial life is fundamental for the ecosystem – more complex life forms in soil and water depend on the activity of microbes – and for the human body – our guts contain enormous numbers of microorganisms necessary to protect us and even to produce vitamins.
“Understanding how pathogens operate can provide additional weapons to fight them.”
Tackling tuberculosis: exploring if chemicals found in corals can prevent the formation of drug-resistant cells and biofilms that make the disease hard to treat
According to the World Health Organisation, tuberculosis (TB) took the lives of 1.4 million people in 2019 and a further estimated 10 million people fell ill with the infectious disease, which mainly affects the lungs.
There are different forms of TB, some of which are treatable and curable. However, ‘multidrug-resistant tuberculosis’ (MDR-TB) is a form of TB caused by bacteria that does not respond to the most effective first-line anti-TB drugs and in severe cases, it also does not respond to the most effective second-line drugs.
Mycobacterium tuberculosis (M. tb) – the pathogenic bacteria that causes TB – can develop this resistance to antibiotic therapy by producing drug-tolerant cells known as ‘persister cells’ and it can form biofilms inside the lungs, as well as on the surfaces of medical devices, that are abundant with these cells.
Bacterial persistence coupled with biofilm formation is directly associated with failure of antibiotic treatment of TB.
Loughborough’s Professor Andrei Malkov, an expert in organic chemistry, is working with biologists and chemists to find molecules capable of inhibiting persister cell and biofilm formation in the hope it will lead to more effective antitubercular therapies.
He said one of the team’s recent successes is the identification and synthesis of chemical compounds found in a species of soft coral that, during in vitro experiments exhibited the ability to inhibit persister cell formation and eradicate biofilms formed by M. tb pathogens.
The team, led by the Russian Academy of Sciences, have submitted a paper on the topic to Cell Chemical Biology and are currently revising the manuscript according to reviewers’ comments.
Professor Malkov commented: “We have identified a small molecule that inhibited formation of biofilms in the laboratory settings.
“This may serve as a promising new lead compound for developing novel antitubercular therapies relying on the suppression of persister cell formation and thus effective against chronic and recalcitrant tuberculosis infections.”
Developing a rapid, easy, and affordable point-of-care test to detect wound infection
Chronic or non-healing wounds, such as in people suffering from diabetes or burns, is a severe healthcare problem.
Interpreting whether a wound is going to heal or lead to a diseased state is a complex problem and as a result it is hard to determine the best course of treatment.
Biofilms are the fundamental reason that chronic wounds do not heal in a timely manner and they form when microorganisms – most commonly bacteria - adhere themselves to the wound surface.
However, bacteria can colonise on wounds without causing an infection, so developing a test to simply get a ‘yes/no’ answer for the presence of bacteria is not massively beneficial.
Dr Sourav Ghosh, a healthcare engineering expert, and PhD student Praveen Kumar Kaveri are developing a rapid, simple, single-step fluorescence-based test that aims to provide crucial information on wound pathogenesis, i.e. whether a wound will heal easily or become non-healing.
The test aims to detect wound infection by determining the number and type of bacteria in a biofilm – known as the ‘bacterial load’ – and then determine the virulence of the bacteria [its ability to prevent wound healing and cause damage to the host].
Dr Ghosh says the research team have had promising results so far and have been able to rapidly detect bacteria quantitatively from a wound mimic sample and confirm at the same time if it is a gram-negative or a gram-positive species, which would help the clinicians in better treatment selection.
In addition, the team have had successes in quickly determining the efficacy of different antimicrobial dressings in killing bacteria.
A paper on the test and the team’s results is expected to be published in early 2021.
“Our research could potentially lead to the creation of the first rapid near-patient test for holistic assessment of wound – bacterial load and infection state – allowing timely and evidence-based optimal management, saving significant costs”, said Dr Ghosh.
“Such a test would also allow the majority of wound care and management load to be transferred from a more expensive hospital-based setting to home and primary care settings.
“Besides reducing the healthcare load, this will also allow us as a society to take better care of the frail and the elderly, particularly during this new-age pandemic situations.”
For more on the NBIC campaign, click here.
This article was written by Megan Cox and is published in VOLUME, Loughborough University’s online magazine





Poll: Should the UK’s railways be renationalised?
The term innovation is bandied about in relation to rail almost as a mantra. Everything has to be innovative. There is precious little evidence of...