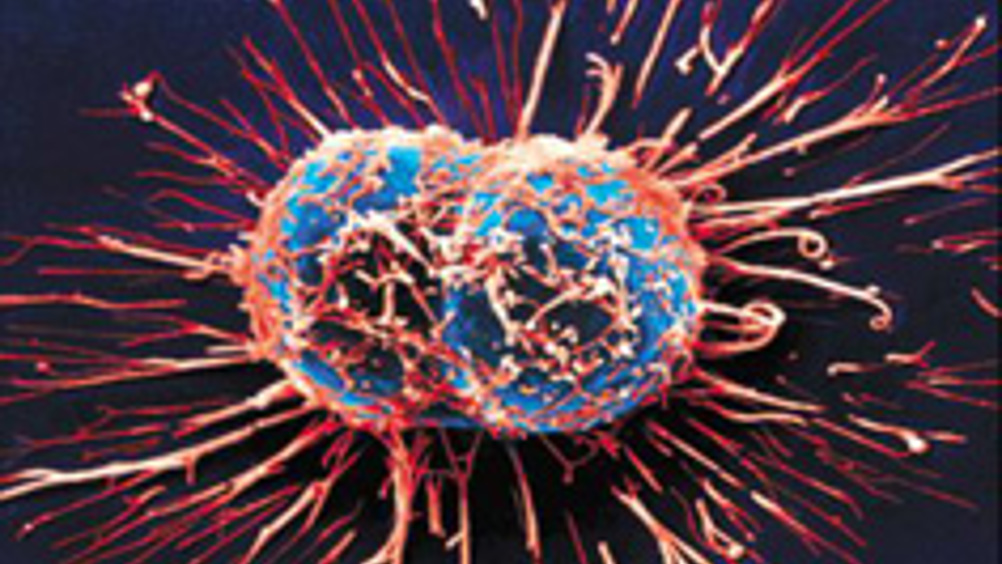
Cancer therapy causes 'avalanche of cell death'
A new type of cancer treatment based on photo-immune therapy has been shown to completely shut down blood supply to tumours, leading to an ‘avalanche of cell death’.
Antibody drugs that stop new vessels forming in tumours have already been developed and marketed — but generally tumours can adapt and rely on back-up mechanisms to get blood flowing again.
A team from Hull University and ETH Zurich have now joined these antibodies to a photosensitive molecule.
The drug is administered intravenously as normal and is localised to the tumour site by the antibody, which attaches to a protein specific to the blood vessels there. The antibody stops the growth of new vessels — but, in addition, light is applied to the tumour, which activates the photosensitive molecule and leads to a cascade that damages existing vessels.
‘The photosensitiser absorbs red wavelength light and it goes into an excited state, so it’s got to get rid of that energy somehow and the way it does that is to interact with oxygen, converting it to something much more cytotoxic — which is bad for any cells in the immediate environment,’ Dr Ross Boyle of Hull told The Engineer.
Register now to continue reading
Thanks for visiting The Engineer. You’ve now reached your monthly limit of news stories. Register for free to unlock unlimited access to all of our news coverage, as well as premium content including opinion, in-depth features and special reports.
Benefits of registering
-
In-depth insights and coverage of key emerging trends
-
Unrestricted access to special reports throughout the year
-
Daily technology news delivered straight to your inbox










Simulations show Optimal Design for Bladeless Wind Turbines
"an 80cm mast" Really? I'm short but that's only half my height! Do they mean 800cm?