In a paper published in Science Advances, the researchers from Nanyang Technological University, Singapore (NTU Singapore) and the Agency for Science, Technology and Research (A*STAR) showed that bringing together two magnets to pinch and apply pressure to a fold of skin led to short term changes in the skin barrier, and specifically the formation of micropores underneath its surface.
Microneedles offer pain-free alternative to hypodermic jabs
In tests on mice, they showed that these micropores, of about three micrometres in area, allowed drugs applied on the surface of the skin to diffuse through it more easily. Six times greater quantity of drug diffused through the skin of mice with the micropores compared to the skin of mice which did not receive the temporal pressure treatment.
“Our research project was first inspired by the traditional Chinese medicine ‘tuina’ therapy, where physicians rub and apply pressure on skin and muscle tissue and apply a topical ointment,” said lead author Dr Daniel Lio.
Experimental results showed that nanoparticles and insulin were effectively delivered through the skin of mice at molecular masses up to 20,000 daltons. This mass is 40 times the largest currently reported in the scientific literature for transdermal drug delivery via microneedle patches, which is 500 daltons.
In experiments, the team also found that with their method, cells in the epidermis were observed to have an increase in the number of so-called gap junctions and a reduction in tight junctions. These junctions control the amount of molecules being delivered between the cells: if there is an increased expression of gap junctions, more molecules can be delivered across the cell barrier, while tight junctions restrict the extracellular movement of molecules.
In the animal experiments, two magnets were used to apply pressure on the mouse dorsal skin for one or five minutes, depending on how fast the drug delivery is needed, before being removed and the drug applied like a cream.
The drug was then left for 12 hours before the skin was imaged with fluorescent microscopy to see to what extent the drug had penetrated through the skin.
The team compared three types of skin: skin that received pressure treatment, skin which had not, and skin which had drugs delivered through microneedles.
Skin that received pressure treatment had similar amounts of drug delivered through the skin to that found with a microneedle patch, while skin that did not receive the pressure treatment had significantly less drug delivered.
Micropores were also observed to disappear a day after they were formed, which suggests that the skin cells have filled up the gaps.
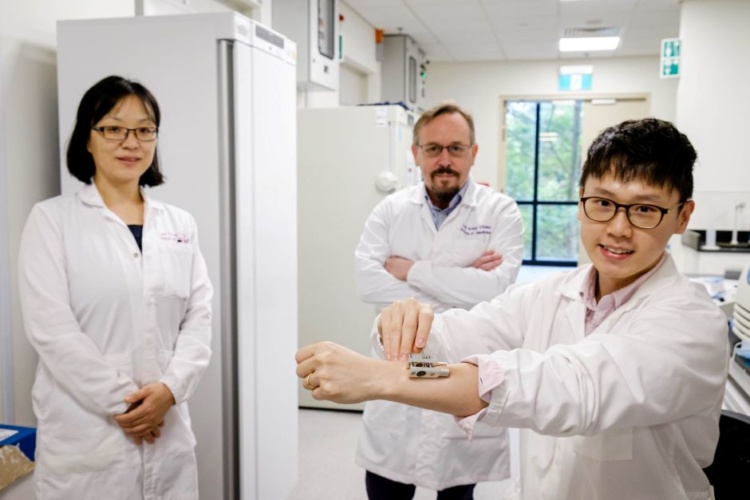
The team has filed a patent for a pressure device through NTU’s innovation and enterprise company, NTUtive, and is carrying out further experiments to refine the drug delivery mechanism.




Poll: Should the UK’s railways be renationalised?
I think that a network inclusive of the vehicles on it would make sense. However it remains to be seen if there is any plan for it to be for the...