Developed by a team of engineers and doctors at the University of Michigan, it could help doctors diagnose and treat cancer more effectively.
"Nobody wants to have a biopsy. If we could get enough cancer cells from the blood, we could use them to learn about the tumour biology and direct care for the patients. That's the excitement of why we're doing this," said Daniel F. Hayes, M.D., the Stuart B. Padnos Professor of Breast Cancer Research at the University of Michigan Rogel Cancer Center and senior author on the paper in Nature Communications.
According to the University of Michigan, tumours can release over 1,000 cancer cells into the bloodstream in a single minute. Current methods of capturing cancer cells from blood rely on samples from the patient - usually no more than a tablespoon taken in a single draw. Some blood draws come back with no cancer cells, even in patients with advanced cancer, and a typical sample contains no more than 10 cancer cells.
Over a couple of hours in the hospital, the new device could continuously capture cancer cells directly from the vein, screening much larger volumes of a patient's blood. In animal tests, the chip in the wearable device trapped 3.5 times as many cancer cells per millilitre of blood as it did running samples collected by blood draw.
"It's the difference between having a security camera that takes a snapshot of a door every five minutes or takes a video. If an intruder enters between the snapshots, you wouldn't know about it," said Sunitha Nagrath, Ph.D., associate professor of chemical engineering at U-M, who led the development of the device.
Research shows that most cancer cells can't survive in the bloodstream, but those that do are more likely to start a new tumour. Typically, it is these satellite tumours, called metastases, that are deadly. Cancer cells captured from blood could therefore provide better information for planning treatments than those from a conventional biopsy.
The team tested the device in dogs at the Colorado State University's Flint Animal Cancer Center where they injected healthy adult animals with human cancer cells, which are eliminated by the dogs' immune systems over the course of a few hours.
For the first two hours post-injection, the dogs were given a mild sedative and connected to the device, which screened between 1-2 per cent of their blood. At the same time, the dogs had blood drawn every 20 minutes, and the cancer cells in these samples were collected by a chip of the same design.
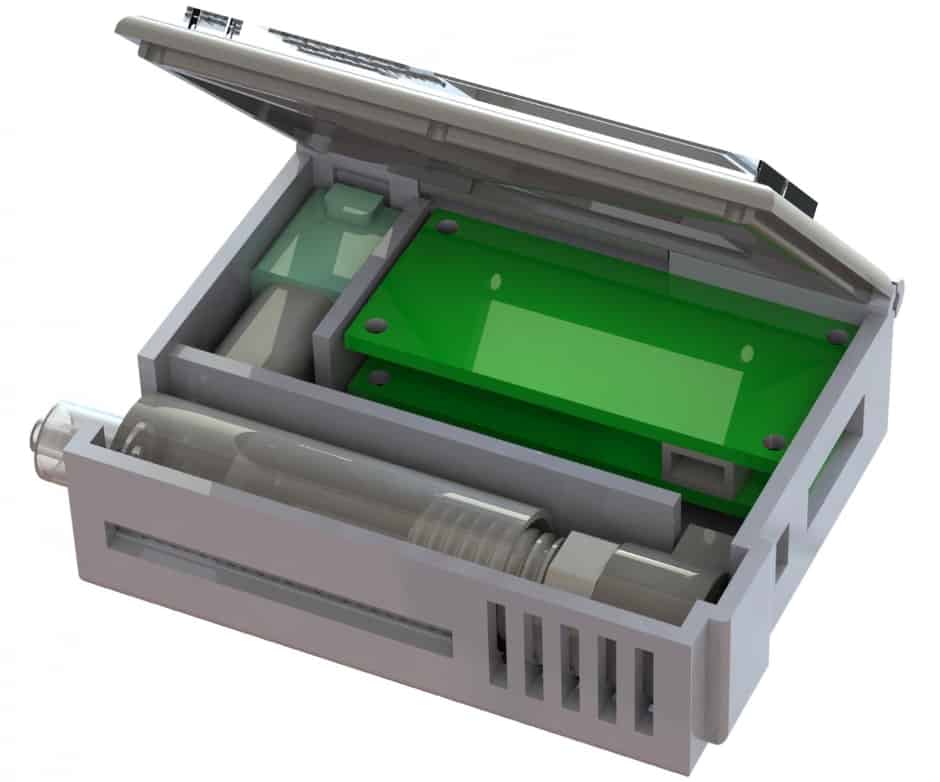
The device itself shrinks a machine that is typically the size of an oven down to something that could be worn on the wrist and connected to a vein in the arm.
"The most challenging parts were integrating all of the components into a single device and then ensuring that the blood would not clot, that the cells would not clog up the chip, and that the entire device is completely sterile," said Tae Hyun Kim, Ph.D., who earned his doctorate in electrical engineering in the Nagrath Lab and is now a postdoctoral scholar at the California Institute of Technology.
They developed protocols for mixing the blood with heparin, a drug that prevents clotting, and sterilisation methods that killed bacteria without harming the cell-targeting immune markers, or antibodies, on the chip. Kim also packaged some of the smallest medical-grade pumps in a 3D-printed box with the electronics and the cancer-cell-capturing chip.
The chip itself uses graphene oxide to create dense forests of antibody-tipped molecular chains, enabling it to trap more than 80 per cent of the cancer cells in whole blood that flows across it. The chip can also be used to grow the captured cancer cells, producing larger samples for further analysis.




Plasma technique converts landfill methane to jet fuel
Trevor; there are still many landfill sites in the UK where the methane is not captured but not only that, where there is protein waste in them, they...