Glucose monitor now available on the NHS is diabetes ‘game changer’
Researchers who carried out an independent study on a new type of glucose monitor, which is now available on prescription in the UK, have hailed it as a major step in the fight against diabetes.
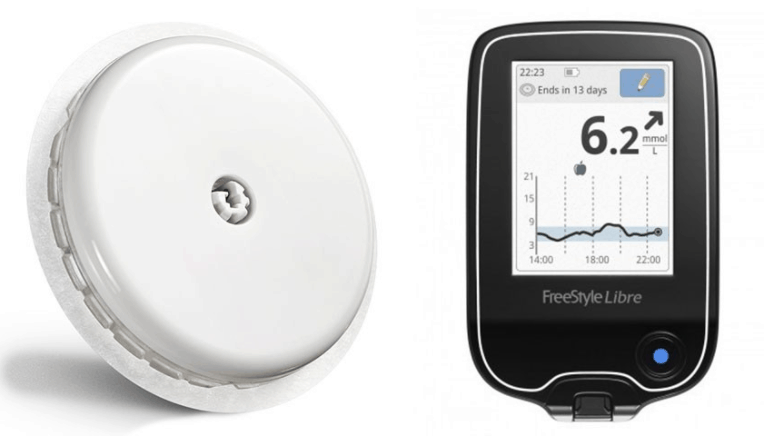
The FreeStyle Libre flash glucose monitor attaches to the upper arm and can measure blood sugar for up to 14 days. When the sensor is applied, a thin, flexible and sterile fibre is inserted just under the skin and held in place with a small adhesive pad. The small disc is designed to replace the 4-10 finger pricks Type 1 diabetes patients need to self-administer daily.
Up to eight hours of glucose data can be stored locally on the waterproof sensor, with a specialised reader used to scan the information in just one second. This data then plugs into a software system that can generate detailed reports on glucose levels, helping users and medical professionals spot patterns of spikes and lows.
“Despite major progress in the care of people living with Type 1 diabetes, many fail to achieve their target blood sugar level – and that risks major complications,” said Dr Lalantha Leelarathna, a researcher from Manchester University and a consultant diabetologist at Manchester Royal Infirmary, Manchester University NHS Foundation Trust.
Register now to continue reading
Thanks for visiting The Engineer. You’ve now reached your monthly limit of news stories. Register for free to unlock unlimited access to all of our news coverage, as well as premium content including opinion, in-depth features and special reports.
Benefits of registering
-
In-depth insights and coverage of key emerging trends
-
Unrestricted access to special reports throughout the year
-
Daily technology news delivered straight to your inbox










Water Sector Talent Exodus Could Cripple The Sector
Maybe if things are essential for the running of a country and we want to pay a fair price we should be running these utilities on a not for profit...