
There are never enough effective cancer therapies, it seems. The challenge of treating a disease that’s essentially the body turning on itself has occupied the medical sector for much of the last half-century. No longer is a cancer diagnosis an automatic death sentence. But the problem remains: how do you kill off the invasive mutant cells of a tumour without damaging healthy surrounding tissue?
It might seem illogical that the answer could lie with nuclear fusion, but fusion depends on particle physics, and such fundamental science has often proved key to the radiotherapy side of cancer treatment. Treatments such as intense X-ray radiation of tumours, nuclear medicine and proton beam therapy all arose from studies of the fundamental composition and behaviour of matter and of electromagnetic radiation.
For California-based TAE Technologies, cancer treatments are a goal with twin advantages. The first, as Bruce Bauer, chief executive of its subsidiary TAE Life Sciences explained to The Engineer, is simply that it offers the opportunity to treat previously intractable forms of the disease. The second is that it allows the parent company, which has a forward-looking and unusual approach to nuclear fusion, to generate income from its technologies before they reach fruition in the energy-generation sector.
“Like most technically heavy research programmes, there’s technology that gets developed along the way that has collateral applications,” Bauer said. In this case, the key technology is a compact particle accelerator.
_____________________________________________________________________________
Further reading
- Proton beam therapy comes of age
- Tracing the sources of nuclear fusion
- Rotherham set for new £22m fusion research centre
_____________________________________________________________________________
Previously known as Tri-Alpha Energy, TAE Technologies is pursuing fusion via a method known as aneutronic power. Whereas in most forms of fusion, the energy of the key reaction is transmitted by emission of fast (i.e. high-energy) neutrons, in aneutronic power the energy is carried by charged particles.
Like many types of fusion reaction, this takes place in a plasma, a cloud of gas composed of charged particles, and this plasma must be heated to encourage its constituent particles to move faster and thus promote fusion-producing collisions. To do this, neutral particles have to be injected into the plasma, and it is this process that gave rise to the key technology that Bauer’s subsidiary is using: a so-called ‘tandem accelerator’ that generates fast neutrons.

“What we’ve done is take tandem accelerator design and repurposed it, downsized it to a much lower power level, and are using it to generate a neutron beam for cancer care,” he said.
The neutron beam is instrumental to a form of treatment that has been investigated in recent decades, but only at a very small number of locations. Boron neutron capture therapy (BNCT) involves directing a beam of high-energy neutrons at a tumour that has previously been infused with a boron 10-containing drug called Boronophenylalanine (BPA). The boron in this compound, which is not radioactive, can capture fast neutrons, and when it does, it breaks down to emit an alpha particle, a lithium nucleus and 2.31MeV of energy. This kills tumour cells but is stopped by cell walls so cannot damage adjacent healthy tissue.
Although BNCT has been studied since the 1960s, the problem with turning it into a clinically available cancer treatment has been the availability of neutron beams. These are very difficult to produce because, being uncharged, neutrons are difficult to accelerate. The only place where a neutron beam has been available is a specialised research reactor.
“At their height, there might have been 10 or 12 of these reactors worldwide that were used,” Bauer said. The most prolific work was in Japan, Taipei and Helsinki, but the Finnish reactor was shut down eight years ago. The Taipei facility is due to be decommissioned next year. “And as you can imagine, a nuclear reactor was never exactly the most convenient, proper, place to treat patients,” Bauer said. “Although over the years, close to 2,000 patients with recurring cancers have been treated with the technique, it’s never been a clinical procedure, only ever research.”
The tandem accelerator gets around the neutron acceleration problem by not accelerating neutrons: it generates fast neutrons within its mechanism by electrostatically accelerating protons so that they collide with a lithium target. The collisions between fast protons and lithium nuclei ejects a stream of energetic neutrons that is suited to BNCT.
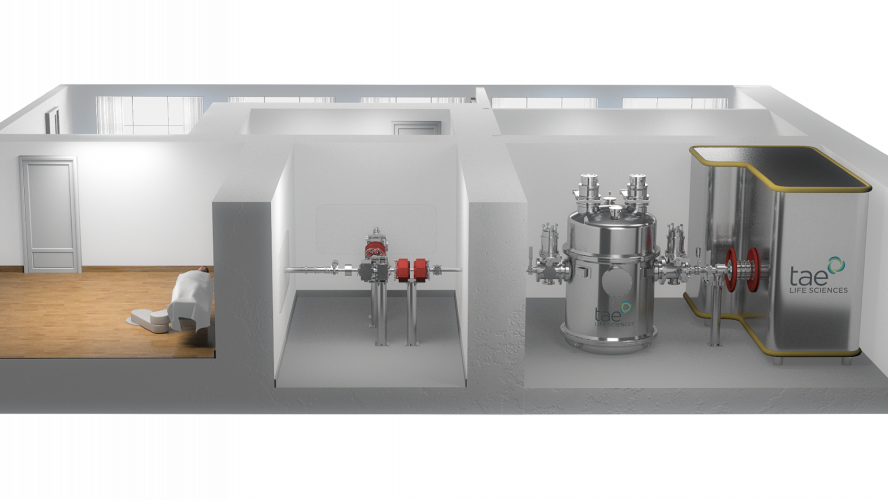
“When you have a tandem design, it enables a relatively compact, small footprint,” Bauer explained. “It’s a very reliable design because you’re using a lower voltage to generate the acceleration. It’s a device that has a form that’s practical to install and operate in a clinical setting: you can put this in the basement hospital quite well. Our target design and beam-shaping assembly comes together into a reasonably compact set-up that can be installed in a vault or a bunker in a hospital. It’s a baby version of what you would expect to see, say, for a proton-beam therapy treatment centre. The shielding is far more modest than for a proton beam.”
TAE is not the only company treading this path, Bauer said. Japan is leading the field, and Finland is also looking at ways to extend its research capabilities beyond the closure of its reactor. But TAE is looking to China for its first exploitations of its version of the technology. “We are partnering with a Chinese company called New Boron, and our first system is going into China at the end of this year,” he said. “We’ll be hoping to treat our first patients sometime early in 2020 and start producing data to go along with Japanese and Finnish groups.”
The choice of China is not just because its huge population means there are likely to be more people with the types of cancer that respond best to BNCT, Bauer explained. The technique seems to be most useful for head and neck cancers, which are difficult to treat by other means, partly because of their proximity to so many vital anatomical structures. “China has five times the incidence of head and neck cancers compared to Europe or the US. They seem to have a perfect storm of risk factors – 16 or 17 per cent of all tumours there fall into that category; elsewhere, it’s more like 3 to 3.5 per cent. It is most likely that there are lifestyle risk factors: many more people smoke, and they eat a lot of food that has been processed with nitrites or smoked, which have been associated with cancer risk. Moreover, there is a high prevalence of human papillomavirus in the population and that’s a known precursor to head and neck cancer. So, there tends to be many more people suffering from those difficult-to-treat cancers.”
"With BNCT, the procedure is only given once or sometimes twice for half an hour or so. The only side-effect really is failure to treat."
Previously, the first-line treatment for this type of tumour is radiotherapy, but this is arduous. “The radiation has to be given in many fractions, 30 times over six weeks. You come back every day. You inevitably damage healthy tissue as well, and that gives rise to side-effects. With BNCT, the procedure is only given once or sometimes twice for half an hour or so. The tumour tissue is subjected to very high levels of destructive energy, but that only happens where you have boron and neutron together at the same time. It’s a highly effective treatment, because it is very damaging to the cell. It causes a very messy double-strand break of the DNA, but it stays inside the cell and an adjacent non-cancerous cell that has no boron in it will be completely untouched. The only side-effect really is failure to treat, perhaps because the tumour is too deep for the neutron beam to reach the target, or the targeting drug hasn’t been effective at getting the boron sufficiently distributed throughout the tumour cells. BPA is a modified form of an essential amino acid, and because cancer cells are perpetually growing and dividing, they have a higher propensity to take it up than healthy cells. You tend to have more than three times as much BPA in a cancer cell. Development work is concentrating on improving the take-up rate, and it would be good for it to persist for 24 to 48 hours so that you could give an infusion one day and bring the patient back the next for the neutron beam treatment. Currently, it has to be within a few hours.”
BNCT has also shown promising results with other types of cancer such as lung and pancreas, where recurrence is common and treatment difficult. Bauer, whose background is in the discipline of biomedical engineering and the business of venture finance, lost his business partner to glioblastoma (an aggressive form of brain cancer) at the age of 60. “It’s very satisfying to me just to be part of a corporate infrastructure that is trying, whether through energy or healthcare, to make an impact on our world,” he said.




Nanogenerator consumes CO2 to generate electricity
Nice to see my my views being backed up by no less a figure than Sabine Hossenfelder https://youtu.be/QoJzs4fA4fo